Malaria është një sëmundje e rrezikshme që transmetohet te njerëzit nga disa lloje mushkonjash. Zakonisht sëmundja regjistrohet në vendet tropikale. Është i parandalueshëm dhe i shërueshëm.
Infeksioni shkaktohet nga një parazit dhe nuk përhapet nga personi në person.
Simptomat mund të jenë të lehta dhe jashtëzakonisht të rënda dhe kërcënuese për jetën. Simptomat e lehta përfshijnë ethe, të dridhura dhe dhimbje koke. Simptomat e rënda përfshijnë lodhje dhe dobësi ekstreme, konfuzion, konvulsione dhe gulçim
Foshnjat, fëmijët nën 5 vjeç, gratë shtatzëna, udhëtarët dhe njerëzit me HIV ose AIDS kanë rrezikun më të lartë të sëmundjes së rëndë.
Ekzistojnë disa metoda për parandalimin e sëmundjes: shmangia e pickimit të mushkonjave, kimioprofilaksia parandaluese dhe vaksinimi. Trajtimi në kohë ndihmon në parandalimin e zhvillimit të një forme të rëndë të sëmundjes.
Malaria zakonisht transmetohet te njerëzit përmes pickimit të mushkonjave femra të infektuara Anopheles . Infeksioni është gjithashtu i mundur përmes transfuzioneve të gjakut dhe gjilpërave të injektimit të kontaminuara. Simptomat e para të sëmundjes mund të jenë të lehta dhe është e vështirë të diagnostikosh malarinë në këtë fazë, sepse mund të ngatërrohet me sëmundje të tjera të shoqëruara me temperaturë. Pa trajtim, malaria e shkaktuar nga P. falciparum mund të përparojë në sëmundje serioze dhe të çojë në vdekje brenda 24 orëve.
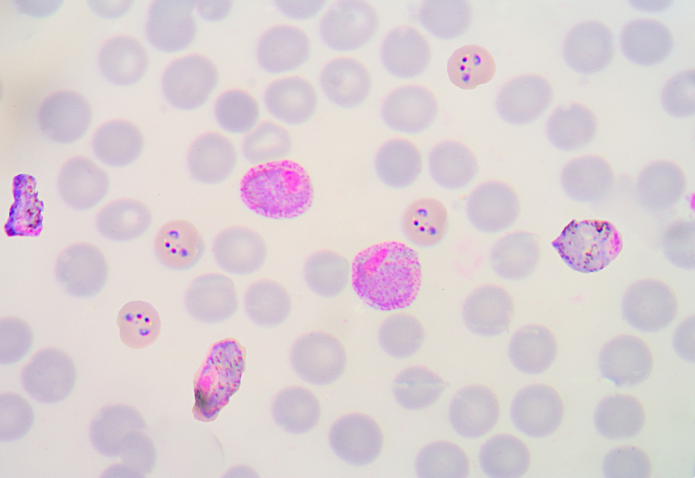
Ekzistojnë 5 lloje të parazitëve Plasmodium që shkaktojnë malarien tek njerëzit. 2 prej tyre – P. falciparum dhe P. vivax – janë më të rrezikshmit. P. falciparum është paraziti më i rrezikshëm i malaries dhe është më i zakonshmi në kontinentin afrikan. P. vivax është paraziti dominues i malaries në shumicën e vendeve jashtë Afrikës Sub-Sahariane. Lloje të tjera që mund të infektojnë njerëzit janë P. malariae, P. ovale dhe P. Knowlesi.
Simptomat më të zakonshme të hershme të malaries janë ethe, dhimbje koke dhe të dridhura.
Simptomat zakonisht zhvillohen brenda 10-15 ditëve pas pickimit nga një mushkonjë e infektuar.
Simptomat mund të jenë të lehta, veçanërisht te njerëzit me një histori të malaries. Për shkak se disa simptoma të malaries janë jo specifike, testimi i hershëm është i rëndësishëm.
Disa lloje të malaries mund të çojnë në sëmundje të rënda dhe madje edhe në vdekje. Foshnjat, fëmijët nën 5 vjeç, gratë shtatzëna, udhëtarët dhe njerëzit me HIV ose AIDS janë në rrezikun më të lartë të një zhvillimi të tillë. Simptomat serioze përfshijnë:
Njerëzit me simptoma të rënda duhet të marrin menjëherë kujdes mjekësor të kualifikuar. Trajtimi në kohë i malaries së lehtë mund të parandalojë përkeqësimin e simptomave, sëmundje të rënda dhe vdekje.
Malaria gjatë shtatzënisë mund të çojë në lindje të parakohshme ose në peshë të ulët të lindjes.
Sipas Raportit Botëror të Malaries, kishte 247 milionë raste të malaries në vitin 2021, krahasuar me 245 milionë raste në vitin 2020. Numri i përgjithshëm i vdekjeve për shkak të malaries vlerësohet në 619,000 në 2021, krahasuar me 625,000 në 2020.
Rajoni afrikan i OBSH-së vazhdon të mbajë barrën më të madhe të sëmundjeve në krahasim me rajonet e tjera. Në vitin 2021, ky rajon përbënte rreth 95% të të gjitha rasteve të malaries dhe 96% të të gjitha vdekjeve nga malaria. Rreth 80% e vdekjeve nga malaria në rajon ndodhin tek fëmijët nën 5 vjeç.
Katër vende afrikane përbëjnë më shumë se gjysmën e vdekjeve nga malaria në botë: Nigeria (31.3%), Republika Demokratike e Kongos (12.6%), Republika e Bashkuar e Tanzanisë (4.1%) dhe Nigeri (3.9%).
Malaria mund të parandalohet duke parandaluar pickimin e mushkonjave të infektuara, duke marrë medikamente të caktuara dhe duke u vaksinuar (aktualisht, vaksina është e disponueshme vetëm për grupmosha të caktuara në 12 vende afrikane). Konsultohuni me mjekun tuaj për marrjen e barnave antimalariale përpara se të udhëtoni në një zonë endemike të malaries .
Ju mund të zvogëloni rrezikun e infeksionit të malaries duke shmangur pickimin e mushkonjave.
Kontrolli i vektorit është komponenti më i rëndësishëm i kontrollit të malaries, sepse është jashtëzakonisht efektiv në parandalimin e infeksionit dhe reduktimin e transmetimit të virusit. Dy metodat kryesore të kontrollit të vektorit janë rrjetat e mushkonjave të trajtuara me insekticide (ITN) dhe spërkatjet e insekticideve me veprim përfundimtar të brendshëm (ILSP).
Progresi në luftën kundër vektorëve të malaries mund të ngadalësohet nga rezistenca e zhvilluar kohët e fundit e mushkonjave Anopheles ndaj insekticideve. Kërcënime të tjera për përdorimin efektiv të metodave të kontrollit të vektorit janë aksesi i pamjaftueshëm në OIS, konsumimi i shpejtë i tyre gjatë përdorimit, si dhe një ndryshim në sjelljen e mushkonjave: sipas disa të dhënave, ekziston një tendencë për të zhvendosur aktivitetin e tyre në një kohë më të hershme, kur njerëzit nuk janë ende në shtëpi, kështu që insektet është e mundur për të shmangur veprimin e insekticideve.
Udhëtarët në zonat endemike të malaries duhet të konsultohen me një mjek disa javë përpara udhëtimit. Një profesionist mjekësor do të përcaktojë se cili ilaç është i përshtatshëm për ju për të parandaluar sëmundjen në varësi të vendit ku do të shkoni. Në raste të caktuara, kemoprofilaksia duhet të fillohet 2-3 javë para nisjes. Ilaçet duhet të merren sipas skemës së përcaktuar gjatë gjithë kohës së qëndrimit në zonën endemike, si dhe brenda 4 javëve nga momenti i kontaktit të fundit të mundshëm me mushkonjat e infektuara, sepse gjatë kësaj kohe paraziti lirohet nga. mëlçinë.
Që nga viti 2019, vendet afrikane si Gana, Kenia dhe Malawi kanë marrë vaksinën e parë në botë për malarinë falë Programit të Zbatimit të Vaksinës së Malaries (MVIP), të koordinuar nga OBSH dhe financuar nga Aleanca e Vaksinave Gavi, Fondi Global për Luftën kundër SIDA-s, Tuberkulozit dhe Malaria, si dhe Unitaid. Vaksina RTS,S/AS01 është administruar te më shumë se 1.7 milionë fëmijë dhe ka demonstruar siguri dhe efikasitet: programi pilot i vaksinimit rezultoi në një reduktim të ndjeshëm të malaries së rëndë dhe vdekjeve tek fëmijët. Të paktën 28 vende afrikane kanë shprehur interes për marrjen e kësaj vaksine. Pra, nga tetori 2021 OBSH rekomandon përdorimin e gjerë të vaksinës së malaries RTS,S/AS01 tek fëmijët që jetojnë në zona me transmetim të moderuar dhe të lartë të malaries P. falciparum . Vaksina ka vërtetuar aftësinë e saj për të reduktuar ndjeshëm incidencën e malaries, veçanërisht formën fatale të malaries, tek fëmijët e vegjël.
Në periudhën 2023–2025 Falë përpjekjeve të Aleancës së Vaksinave Gavi (Gavi), Organizatës Botërore të Shëndetësisë (OBSH) dhe Fondit Ndërkombëtar të Fëmijëve të Kombeve të Bashkuara (UNICEF), 12 vendet në Afrikë që kanë më shumë nevojë për vaksinën për parandalimin e malaries do të marrin 18 milionë doza . Vendet e Programit të Zbatimit të Vaksinës së Malaries (MVIP) – Gana, Kenia dhe Malavi – do të marrin vaksinën për të vazhduar projektin pilot të vaksinimit që ka nisur atje që nga viti 2019. Gjithashtu, 9 vende afrikane si Benini, Burkina Faso, Burundi, Kameruni, Republika Demokratike e Kongos, Liberia, Nigeri, Sierra Leone dhe Uganda do të marrin vaksinën për herë të parë.
“Kjo vaksinë ka potencialin të ndikojë ndjeshëm në situatën e incidencës së malaries; përdorimi i tij së bashku me masat e tjera parandaluese mund të parandalojë dhjetëra mijëra vdekje çdo vit”, thotë Thabani Maphoza, menaxher rajonal i Aleancës së Vaksinave Gavi.
Në tetor 2023, OBSH miratoi vaksinën e dytë të malaries. Vaksina R21 është vaksina e dytë e malaries e rekomanduar nga OBSH pas vaksinës RTS, S/AS01. Të dyja vaksinat janë provuar të jenë të sigurta dhe efektive në parandalimin e malaries tek fëmijët.
OBSH vëren se kërkesa për vaksina kundër malaries është e paprecedentë, por ka mungesë të RTS,S. Shtimi i R21 në listën e vaksinave të malaries të rekomanduara nga OBSH pritet të sigurojë furnizime adekuate të vaksinës për të gjithë fëmijët që jetojnë në zonat ku malaria është një rrezik për shëndetin publik.
“Endërroja ditën kur do të kishim një vaksinë të sigurt dhe efektive kundër malaries. Tani kemi dy prej tyre”, tha Tedros Adhanom Ghebreyesus, Drejtor i Përgjithshëm i OBSH-së.
OBSH thotë se efektiviteti i dy vaksinave është "shumë i ngjashëm" dhe nuk ka asnjë provë që njëra është më e mirë se tjetra.
“Kjo vaksinë e dytë ka potencial real për të mbyllur hendekun e madh midis kërkesës dhe ofertës”, tha drejtori rajonal i OBSH-së për Afrikën, Matshidiso Moeti.
Vaksina R21 është 75% efektive në parandalimin e sëmundjeve në rajonet ku malaria është sezonale. OBSH deklaron se ky efikasitet i lartë është i ngjashëm me atë të demonstruar me administrimin sezonal të RTS,S.
Ndikimi në shëndetin publik i vaksinës R21 pritet të jetë i lartë.
Me një kosto prej 2-4 dollarë amerikanë për dozë, kosto-efektiviteti i vaksinës R21 do të ishte i krahasueshëm me ndërhyrjet e tjera të rekomanduara antimalariale, që kërkojnë katër doza për person.
Deri më sot, nuk ka asnjë provë që një vaksinë – R21 ose RTS,S – funksionon më mirë se tjetra. Zgjedhja e një vaksine për përdorim në një vend duhet të bazohet në disponueshmërinë dhe përballueshmërinë e saj.
Provat klinike kanë treguar se vaksina R21 është e sigurt. Ashtu si me vaksinat e tjera të reja, monitorimi i sigurisë do të vazhdojë.
Diagnoza dhe trajtimi në kohë i malaries ndihmojnë në uljen e ashpërsisë së rrjedhës së sëmundjes dhe parandalimin e vdekjes së pacientit, si dhe kontribuojnë në uljen e intensitetit të transmetimit të malaries. OBSH rekomandon që në të gjitha rastet e dyshuara të malaries, të konfirmohet diagnoza me një test diagnostik për zbulimin e parazitit (ekzaminim mikroskopik ose test diagnostik diagnostik).
Malaria është një infeksion serioz dhe kërkon trajtim mjekësor në të gjitha rastet.
Një sërë ilaçesh përdoren për parandalimin dhe trajtimin e malaries. Mjeku përshkruan një ose më shumë barna bazuar në:
Ilaçet më të zakonshme antimalariale janë renditur më poshtë.
Shumica e barnave janë në dispozicion në formën e tabletave. Disa njerëz mund të kenë nevojë për injeksione në një qendër mjekësore ose spital.
Gjatë dekadës së fundit, përpjekjet globale për kontrollin e malaries kanë filluar të pengohen nga zhvillimi i rezistencës së pjesshme të parazitit ndaj barnave me bazë artemisinin në nënrajonin e Mekong-ut të Madh. OBSH është e shqetësuar për raportet e rezistencës së pjesshme ndaj artemisininës në Afrikë, e cila është konfirmuar në Eritrea, Ruanda dhe Ugandë. Për të zhvilluar strategji trajtimi për vendet endemike të malaries, si dhe për zbulimin dhe kontrollin në kohë të rezistencës ndaj ilaçeve, është e nevojshme të kryhet monitorim i rregullt i efektivitetit të barnave antimalariale.
